Abstract
Objective: To characterize, among non-breathing flaccid neonates at delivery, immediate heartrate and responses to ventilation in relation to the clinical diagnosis of fresh stillbirth (FSB) or early neonatal death (END) within 24 hours.
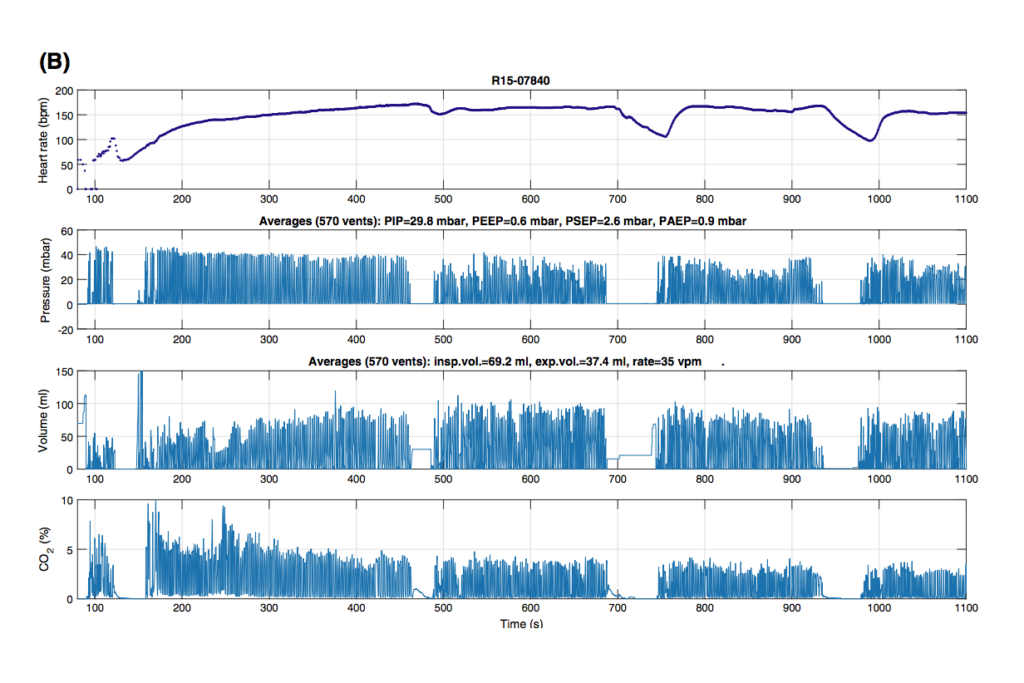
Methods: The present cross-sectional study included all deliveries at Haydom Hospital in rural Tanzania between July 1, 2013, and July 31, 2016. Ventilation parameters and heartrate were recorded by monitors with ventilation and dry-electrocardiography
sensors. Perinatal characteristics were recorded on data forms by trained research assistants.
Results: Among 12 789 neonates delivered, 915 were ventilated; among ventilated neonates, there were 53 (6%) FSBs and 64 (7%) ENDs. Electrocardiography was used in 46 FSBs and 55 ENDs, and these neonates were included in a subanalysis. Initial heartrate was detected in 27 (59%) of 46 FSBs and 52 (95%) of 55 ENDs, and was lower in FSBs (52 ± 19 vs 76 ± 37 bpm; P=0.003). More ENDs responded to ventilation (53% vs 9%; P<0.001), with heartrate increasing above 100 bpm. Heartrate at ventilation discontinuation was higher among ENDs (115 ± 49 vs 52 ± 33 bpm; P<0.001).
Conclusion: Progression to FSB or END after intrapartum hypoxia/anoxia is probably
part of the same circulatory end-process. Distinguishing FSB from severely asphyxiated
newborns is clinically difficult and probably influences estimated global perinatal
mortality rates.
Read the full publication here.