
Learning from experts: Sharing research and supporting collaboration
According to the WHO Progress Report 2023 the reduction of deaths of pregnant women, mothers, and babies has stagnated since 2015.
Research projects in several countries including Tanzania, Nepal, the Democratic Republic of the Congo, Norway, and the United States are focused on research and innovation to improve maternal and newborn health. Over the past three years, these separate research groups have met each month –virtually—as an informal network to share what they’ve learned. Last week they met in person for the first time.
Common interest, common tools
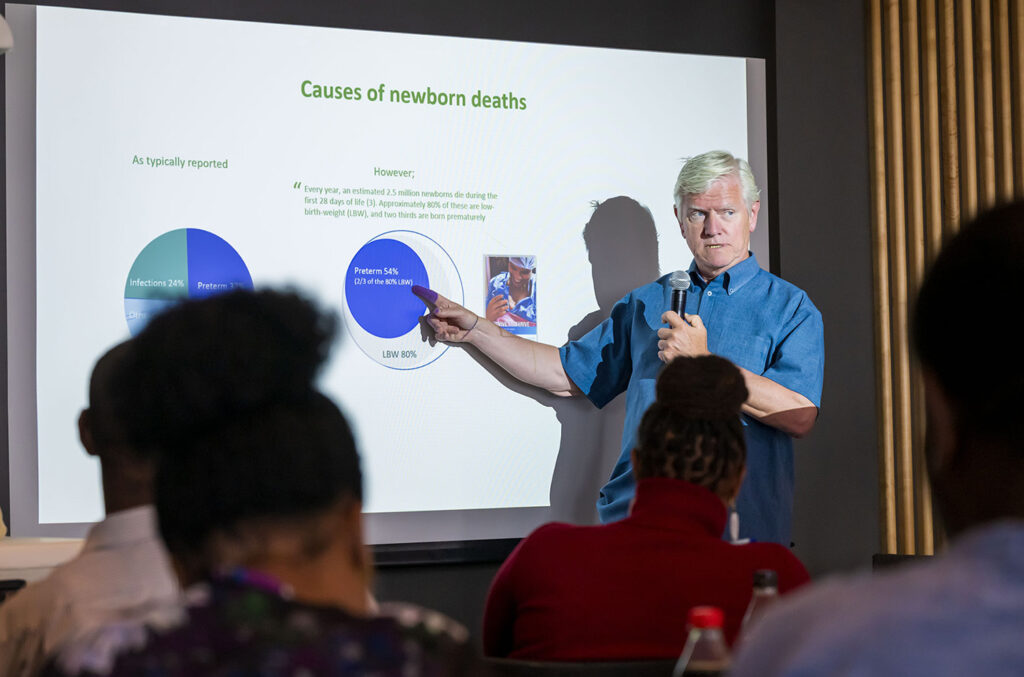
Hosted at the Laerdal headquarters in Stavanger, Norway, by Laerdal’s Strategic Research team, the 1st International Expert Meeting for Safer Births Liveborn research gathered more than 40 international experts to address global challenges related to maternal and newborn mortality and discuss opportunities for collaboration, product development, and new research.
The meeting aimed to build on the innovations developed as a result of Safer Births research and development. The researchers and clinicians who gathered share a common interest— the use of the lifesaving Safer Births innovations and Liveborn tools.
Liveborn is software for data collection, real-time guidance, and post-resuscitation debriefing. Liveborn is used in clinical settings with the heart rate meter, NeoBeat, the fetal heart rate monitor, Moyo and with the NeoNatalie Live simulator in training settings.
Understanding unanswered questions
Globally, neonatal mortality continues to be a challenge as a result of complications during childbirth including asphyxia, prematurity, and infections. While there are demonstrated effective interventions like the Safer Births Bundle of Care (SBBC), there are still important questions to be answered:
- How well can we prevent birth asphyxia in the first place?
- Can we help increase use of vacuum assisted birth to reduce unnecessary c-sections?
- How can we better support clinicians with real-time guidance and clinical debriefing?
- Research + innovation: Contributing to the global research community
The research teams presented ongoing research as well as concepts for clinical, training, and decision-making tools to support Safer Births research collaborations in the years to come.
Tanzania
The Safer Births project was initiated at Haydom Lutheran Hospital in 2012 with a grant from the Norwegian Research Council. Safer Births aimed to reduce maternal and newborn mortality in Tanzania. The research and innovations from this project have been shown to enable each midwife to save two additional lives, every year. These results led to the development of the Safer Births Bundle of Care program which is now scaling up to 110 hospitals in Tanzania.
While SBBC is scaling up proven interventions, new opportunities have been identified for the Safer Births 3 project. With funding support from Innovation Norway, Safer Births 3 focuses on the intrapartum perspective. To address unnecessary c-sections which leads to an increased risk of death to both mother and baby, Haydom Hospital has established the Safe Vacuum project to support decision-making and increase competency of healthcare personnel to ensure safe and timely vacuum assisted births in second stage of labor.
Another research topic is the use of Liveborn Station data to drive simulation-based education at the Stavanger Acute Medicine Foundation for Education and Research (SAFER). Two midwives have started their PhD training at Haydom to study the feasibility and acceptability of Safe Vacuum.
Nepal
The Safer Births innovations were introduced in Nepal in 2018 and scaled up in nine hospitals. Liveborn data was used to study heart rates in crying and non-crying infants and the effect of delayed cord clamping. More recently, researchers investigated the feasibility and acceptability of the use of the Liveborn Station at Bharatpur Hospital. Now, the application of machine learning and artificial intelligence to audio and video signals is being investigated.
The Liveborn Station technology can automatically detect newborn ventilation and provide real-time guidance for healthcare providers. This initiative is called MALA, (Machine Learning Application). A PhD project to study the effect is currently underway at Uppsala University.
“Together, we are building a safer future for mothers and babies during birth, brick by brick.”
— Ashish KC, Nepal

Democratic Republic of the Congo
The Democratic Republic of the Congo (DRC) is the second largest country in Africa with a population of 112 million people. In 2018, a Laerdal Foundation grant for Saving Lives at Birth was awarded to study the effect of the NeoBeat heart rate meter for the management of stillbirth. The study was led by University of North Carolina and Kinshasha School of Public Health together with researchers from Washington, Calgary and the American Academy of Pediatrics. These partners developed the first version of the Liveborn Observation tool to collect research data with NeoBeat.
“This is the only research consortium that develops granular data on newborn resuscitation. It’s such a unique and diverse network.”
– Carl Bose, University of North Carolina
Now, an updated version has been developed and is able to provide real-time guidance and debriefing following newborn resuscitation. This innovation is currently being evaluated at six hospitals in Kinshasha (BIRTH study) with funding support from the National Institute of Health, U.S.A. A parallel program, the LEARN study, is using the Liveborn Station to learn from every birth and resuscitation.
Norway
In collaboration with Haydom Lutheran Hospital, Stavanger University Hospital (SUS) initiated an early study of the use of NeoBeat together with Liveborn observation tool and video. SUS has also studied the effect of low-dose high-frequency (LDHF) training using the NeoNatalie Live simulator. This research is organized under Safer Births Stavanger with 8 PhD generating more than 30 publications. SUS is engaged in machine learning and AI with the NewbornTime project and a new initiative – Safer Births Norway. The goal is to use new technology to enable learning from every resuscitation. SUS is also a partner in the Safe Vacuum project in Tanzania.
University of Stavanger (UiS) researchers have developed machine learning and artificial using data, video, and audio from the SUS, Nepal, Tanzania and DRC research projects. This technology creates timelines for research and debriefing following birth and resuscitation. Together, UiS and Laerdal are testing real-time AI analysis from audio signal data from Nepal as part of the MALA initiative.
Looking forward: New opportunities in Research + Innovation
The aim of the informal Safer Births and Liveborn Expert meeting is to strengthen international collaboration in research and development.
Highlighted themes:
- The opportunity to learn from every birth and resuscitation using Liveborn technology
- Using Safe Vacuum innovations to save lives, time and resources
- To use AI and machine learning to create real-time guidance and timelines at birth
We look forward to the development of new collaborations, new products, and new research contributions to the global community.
Most recent publications:
- Improving Newborn Resuscitation by Making Every Birth a
Learning Event (NCBI) - Delayed and Interrupted Ventilation with Excess Suctioning after Helping Babies Breathe with Congolese Birth Attendants (MPDI)
- Perceptions and experiences of Congolese midwives implementing a low-cost battery-operated heart rate meter during newborn resuscitation (Frontiers)
- Observational study comparing heart rate in crying and non-crying but breathing infants at birth (BMJ)
- Increased risk of bradycardia in vigorous infants receiving early as compared to delayed cord clamping at birth (Nature)
- Usability, acceptability and feasibility of a novel technology with visual guidance with video and audio recording during newborn resuscitation: a pilot study (BMJ)
- Beyond research: improved perinatal care through scale-up of a Moyo fetal heart rate monitor coupled with simulation training in northern Tanzania for helping babies breathe (BMC)
- Fetal to Neonatal Heart Rate Transition during Normal Vaginal Deliveries: A Prospective Observational Study (MPDI)
- Perceptions and experiences of diploma nursing students on clinical learning. A descriptive qualitative study in Tanzania (BMC)
- Use of Pulse Oximetry during Resuscitation of 230 Newborns—A Video Analysis (MPDI)
- Newborns requiring resuscitation: Two thirds have heart rate ≥100 beats/minute in the first minute after birth – Kibsgaard – 2023 – Acta Paediatrica – Wiley Online Library (Wiley)
- Comparison of Heart Rate Feedback from Dry-Electrode ECG, 3-Lead ECG, and Pulse Oximetry during Newborn Resuscitation (MPDI)
- Fetal heart rate development during labour (BMC)
- Newborn Time – improved newborn care based on video and artificial intelligence – study protocol (BMC)
- Towards using Thermal Cameras in Birth Detection (IEEE)
Together with:
- Haydom Lutheran Hospital, Tanzania
- Bharatpur Hospital, Nepal
- Golden Community, Nepal
- Kinshasa School of Public Health, DRC Congo
- Kingasani Hospital, DRC Congo
- University of North Carolina, United States
- Stavanger University Hospital, Norway
- University of Stavanger, Norway
- Laerdal Medical Strategic Research, Norway
- Laerdal Global Health, Norway
- Laerdal Foundation, Norway